Dyspepsia, commonly known as indigestion or “gastric issues”, refers to a group of symptoms that occur in the upper abdomen and often include discomfort or pain, bloating, belching, and nausea.
Dyspepsia can have multiple underlying causes, and identifying the specific factors contributing to an individual’s symptoms may require a thorough evaluation by a trusted doctor.
Treatment typically involves addressing the underlying cause, making dietary and lifestyle modifications, and sometimes using medications to alleviate symptoms.
Here are some common causes of dyspepsia that we see in Paddington Medical.
Dietary Factors
Certain foods and beverages, such as spicy or fatty foods, caffeine, alcohol, and carbonated beverages, can trigger symptoms of dyspepsia in some individuals. Reduction of alcohol, caffiene and spicy foods especially can reduce the symptoms of dyspepsia in a lot of our patients.
Medications
Certain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, antibiotics, and some prescription medications, can irritate the stomach lining and contribute to dyspepsia. Not everyone will experience these side effects of medications, but its prudent to note that
Gastric Acid
Excessive production of gastric acid or the reflux of stomach acid into the esophagus can irritate the stomach lining and lead to symptoms of dyspepsia. Conditions such as gastroesophageal reflux disease (GERD) can cause heartburn and indigestion.
Psychological Factors
Stress, anxiety, and other psychological factors can exacerbate symptoms of dyspepsia or make them more difficult to manage.
Pregnancy
Hormonal changes during pregnancy can affect digestion and lead to symptoms of dyspepsia, particularly during the later stages of pregnancy when the growing uterus puts pressure on the stomach.
Smoking
Smoking cigarettes can increase the risk of dyspepsia by irritating the stomach lining and increasing stomach acid production.
Gastrointestinal Disorders
Various gastrointestinal conditions, such as peptic ulcers, gastritis, gallstones, pancreatitis, gastroparesis (delayed stomach emptying), and irritable bowel syndrome (IBS), can cause symptoms of dyspepsia.
Helicobacter pylori Infection
Infection with the bacteria Helicobacter pylori or H Pylori, is a common cause of chronic gastritis and peptic ulcers, both of which can result in symptoms of dyspepsia.

What is a serious cause of gastric issues that we treat in Paddington Medical? What is Helicobacter Pylori and why is it important for early diagnosis and treatment?
Helicobacter pylori is a type of bacteria that infects the stomach lining, leading to various gastrointestinal conditions. It is important to treat H. pylori infections for several reasons:
Peptic Ulcers
H. pylori is a major cause of peptic ulcers, which are open sores that develop on the inner lining of the stomach or the upper part of the small intestine. These ulcers can cause symptoms such as abdominal pain, bloating, nausea, and vomiting. Treating H. pylori infection can help heal existing ulcers and prevent the recurrence of new ulcers.
Gastritis
H. pylori infection is a common cause of gastritis, which is inflammation of the stomach lining. Chronic gastritis can lead to symptoms such as abdominal pain, indigestion, and loss of appetite. Treatment of H. pylori infection can help reduce inflammation and alleviate symptoms of gastritis.
Reducing the Risk of Gastric Cancer
Long-term infection with H. pylori is associated with an increased risk of developing gastric (stomach) cancer. H. pylori infection can cause chronic inflammation and damage to the stomach lining, which may eventually lead to the development of cancerous cells. Treating H. pylori infection can reduce the risk of gastric cancer by eliminating the underlying cause of chronic inflammation.
Preventing Complications from H. Pylori infection
In addition to peptic ulcers and gastritis, untreated H. pylori infection can lead to other complications, such as gastric bleeding, stomach perforation (a hole in the stomach wall), and gastric outlet obstruction (blockage of the stomach outlet). Treating H. pylori infection can help prevent these serious complications.
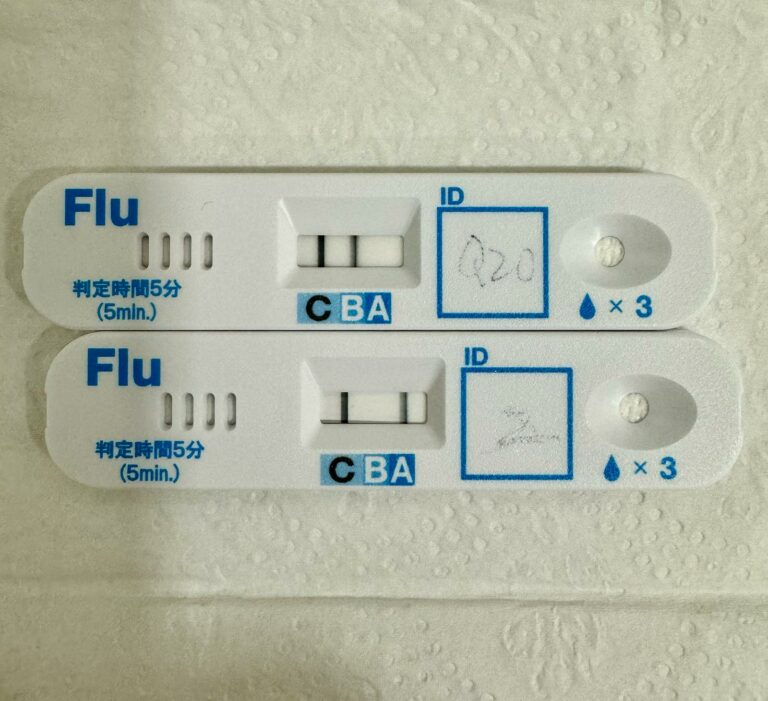
How is Helicobacter Pylori infection diagnosed?
Diagnosing Helicobacter pylori (H. pylori) infection typically involves a combination of non-invasive and invasive tests. Here are some common methods used for screening and diagnosis that can be done in Paddington Medical
Blood Tests for Helicobacter Pylori antibodies
Blood tests can detect antibodies produced by the body in response to H. pylori infection. However, these tests cannot distinguish between current and past infections and may remain positive even after successful eradication of the bacteria. Blood tests are often used as screening tools but may not be reliable for diagnosing active infections.
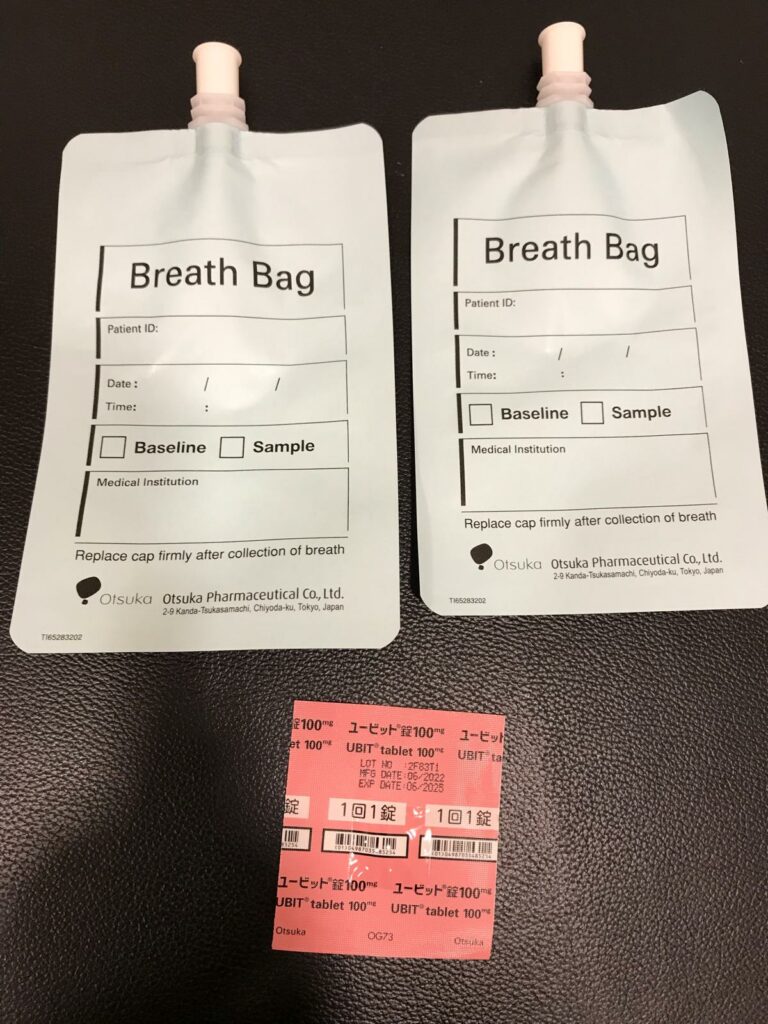
Urea Breath Test (UBT)
UBT is a non-invasive test that measures the presence of special carbon dioxide in the breath after the ingestion of a urea solution. H. pylori produces an enzyme called urease, which breaks down urea into carbon dioxide and ammonia. If H. pylori is present in the stomach, the special carbon dioxide is detected in the breath. UBT is highly sensitive and specific for diagnosing H. pylori infection and can also be used to confirm eradication after treatment.
Endoscopy with Biopsy
Endoscopy involves the insertion of a thin, flexible tube with a camera (endoscope) into the stomach and duodenum. During the procedure, the healthcare provider can visually inspect the stomach lining for signs of inflammation, ulcers, or other abnormalities. Biopsy samples may be taken from the stomach lining for histological examination (microscopic analysis) and testing for H. pylori infection using special stains or molecular methods. Endoscopy with biopsy is considered the gold standard for diagnosing H. pylori infection and is particularly useful for evaluating patients with alarm symptoms (e.g., bleeding, unexplained weight loss) or those requiring treatment for associated conditions such as peptic ulcers or gastric cancer. Paddington Medical works with trusted specialists to do this procedure, if indicated.

How is Helicobacter Pylori treated?
Helicobacter pylori (H. pylori) infection is typically treated with a combination of antibiotics and acid-suppressing medications. The goal of treatment is to eradicate the bacteria, reduce symptoms, promote healing of the stomach lining, and prevent complications such as peptic ulcers and gastric cancer. Treatment regimens may vary depending on factors such as antibiotic resistance patterns, patient tolerance, and local guidelines, but a standard treatment approach via triple therapy in Paddington Medical often involves the following:
Proton pump inhibitor (PPI): Reduces stomach acid production and helps to create an environment that is less favorable for H. pylori survival.
Clarithromycin: An antibiotic that inhibits bacterial growth by interfering with protein synthesis.
Amoxicillin or metronidazole: Another antibiotic that targets H. pylori by inhibiting bacterial cell wall synthesis (amoxicillin) or DNA replication (metronidazole).
Treatment duration typically ranges from 10 to 14 days, but may be extended in cases of treatment failure or in patients with complicated infections. It’s essential for patients to complete the full course of antibiotics as prescribed even if symptoms improve before the treatment is completed.
After completing treatment, follow-up testing is needed to confirm eradication of H. pylori, particularly in patients with peptic ulcers. This may involve repeat urea breath testing, UBT in clinic, If H. pylori is still present after initial treatment, alternative regimens may be considered.
GET IN TOUCH
Schedule a Visit

Dr Lee Joon Loong
Medical Director
MBBS (Australia)
Graduate Diploma in Geriatric Medicine
Designated Workplace Doctor (CAW)
EIMS Primary Care Physician
Certificate Course in Andrology (Men’s Health)
Dr Lee is in Clinic on Monday, Tuesday, Wednesday, Friday, Saturday.
Dr Lee’s surgical procedure days are on Tuesday and Thursday